A pacemaker-like brain device has proved to successfully treat severe depression
Depression has many faces, which is why people dealing with its symptoms have a myriad of different coping mechanisms. For some, it can even be too overwhelming to handle. This was the case of 38-year-old Sarah, who had been living with depression since childhood. As she shared with The New York Times, five years ago, all Sarah could think of was to end her life, “I couldn’t stop crying. The thought that consumed me the entire way on that road was just driving my car into the marshland so I can drown.”
Shortly after this incident, Sarah moved in with her parents because doctors considered it unsafe for her to live alone. No longer able to function at work, she also had to quit her health technology job. Sarah tried nearly every treatment, from different medications and months in a hospital day programme to electroconvulsive therapy and transcranial magnetic stimulation. But just like nearly a third of the more than 250 million people suffering from depression worldwide, her symptoms persisted.
That was until Sarah became the very first participant in an unusual study of an experimental therapy. In a new study published Monday 4 October in Nature Medicine, scientists at the University of California, San Francisco, detailed how their method appears to have successfully treated Sarah. And at a press conference held the week prior, she herself testified to the almost instantaneous relief she experienced after starting the treatment. So what is this near-miraculous cure?
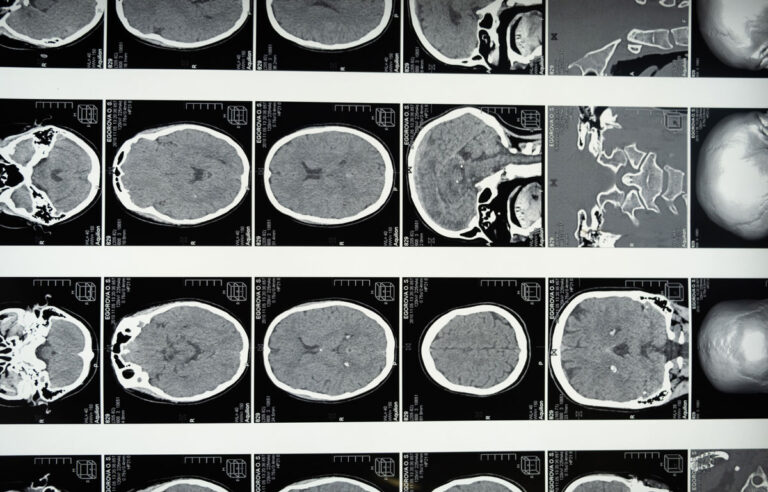
Deep brain stimulation (DBS) is already successfully used to help manage neurological conditions including Parkinson’s disease and certain types of seizures. The concept behind DBS is to transmit electrical impulses to balance out the erratic patterns of brain activity associated with the target condition, hopefully eliminating or reducing a person’s symptoms. These impulses are sent out through electrodes implanted in the brain, which are regulated by a device typically implanted somewhere else in the body, much like how a heart pacemaker works.
When it comes to DBS for depression, it is important to note that there are noticeable differences between the brains of people diagnosed with depression and those who are not. Until now, evidence for the benefits of DBS have been inconsistent, with patients having varying responses to the treatment. That’s why, in recent years, scientists behind the newly published research have been working on ways to improve DBS—such as by finding possibly more relevant areas of the depressed brain to stimulate. Based on that earlier research, they’ve managed to develop their own unique DBS technique which they call “personalised closed-loop neurostimulation.”
The method is said to work by first finding the specific brain activity patterns associated with a patient’s depressive state and then fine-tuning the impulses needed to counteract them. After that’s done, the patient is equipped with a device that can detect when these moments of erratic brain activity show up and automatically send stimulation to the brain. This is different to typical DBS, which involves sending impulses all the time or at fixed intervals of the day.
“In Sarah’s case, the dysfunctional brain activity involved the ventral striatum, a crucial player in decision making, as well as the amygdala, an important regulator of our emotional response, particularly fear and anxiety,” further explained Gizmodo.
And so far so good for the team. “When I first received stimulation, the ‘aha’ moment occurred, I felt the most intensely joyous sensation, and my depression was a distant nightmare for a moment,” said Sarah at the press conference. “The expression made me realise that my depression was not a moral failing. It was a disorder that could be treated, and there was hope for my recovery.”
The authors do caution, however, that this is a single case and that Sarah’s experience should only be seen as a proof of concept for now. It will take more research to see if this treatment can be successfully replicated. And even if it can be, Sarah’s treatment took a lot of resources and time to calibrate—efforts that will make it hard right now for this technology to become widely used by patients with depression. Though the device itself is commercially available, the treatment would still be expensive, with the researchers estimating a cost of about $30,000, based on existing costs for DBS.
As for Sarah, her symptoms of depression did start to return in the time between the first stimulation sessions and the implanting of the permanent device. But once it was implanted and turned on, she again felt immense relief—enough to finally apply the skills she had learned in therapy earlier, she said. Now a year into the treatment, her depression remains at bay and she feels able to “rebuild a life worth living.”





